Connect With Us
Blog

Making Sense of Plantar Fasciitis
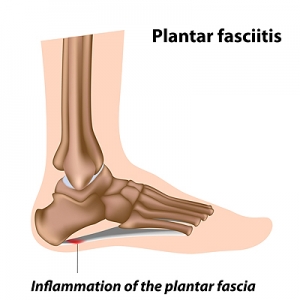
The fascia is a long, fibrous band of tissue that connects the ball of the foot with the heel bone. When that tissue becomes injured or damaged it can tear, and become inflamed and painful. This is a condition known as plantar fasciitis. There are many reasons why plantar fasciitis can occur, including wearing shoes that don’t provide adequate support, having a job that requires you to stand all day, and being obese, old, or very physically active. Certain structural anomalies, like high arches and flat feet, or alignment/gait issues can also contribute to plantar fasciitis developing. A telltale sign of plantar fasciitis is pain that is intense when you first wake up, and then gets gradually better as the day progresses. Since plantar fasciitis is the most common form of heel pain, podiatrists have a great deal of experience treating this condition. They may use rest, ice, physical therapy, night splints, and orthotics to treat it. If these protocols don’t yield optimum results, the podiatrist may use extracorporeal shock wave therapy to heal pain and boost the body’s natural healing process to repair the damaged plantar fascia. If you believe you may have plantar fasciitis, it is suggested that you see a podiatrist for an accurate diagnosis and expert treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Understanding Tarsal Tunnel Syndrome
On the inside of the ankle lies a narrow passageway created by soft tissue and bone, called the tarsal tunnel. Traveling through the tarsal tunnel are tendons, blood vessels, and nerves—including the tibial nerve. This nerve can become compressed within the narrow space of the tarsal tunnel by a variety of conditions that take up space within it. These conditions include lesions or masses, enlarged veins, benign bony growths, and tumors of nerve fibers or ganglion cells. Certain injuries or trauma, as well as having flat feet can contribute to the development of tarsal tunnel syndrome. Tarsal tunnel syndrome can cause pain, tingling, or burning anywhere on the tibial nerve, which runs from the ankle up through the back of the leg. If you believe you may have tarsal tunnel syndrome, schedule an appointment with a podiatrist who will examine you, and may also use nerve tests and imaging to help diagnose the issue. Treatment for tarsal tunnel syndrome may include icing, resting, anti-inflammatory medicines, custom orthotics, and physical therapy. More severe cases may require steroid injections or even surgery to increase space within the tunnel and reduce pressure on the nerve.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
Diabetic Neuropathy and the Feet
Diabetic neuropathy is a type of nerve damage that is caused by high blood sugar levels. Symptoms of diabetic neuropathy most frequently affect the lower limbs and can include pain, numbness, tingling, muscle weakness, and loss of sensation. People with diabetic neuropathy are also at an increased risk of developing diabetic foot ulcers, open wounds on the feet that are difficult to detect (due to a loss of sensation) and that heal slowly and poorly. Other than managing your blood sugar levels, the best way to prevent complications from diabetic neuropathy is to perform daily foot checks. Inspect your feet for any changes, such as cuts, scrapes, sores, wounds, discoloration, pain, or altered sensations. If you notice anything out of the ordinary, seek the care of a podiatrist as soon as possible.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Mark Isenberg, DPM from Center for Podiatric Excellence. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Signs You May Have a Fungal Toenail Infection
A fungal nail infection occurs when the nail is invaded by a fungus. As the fungus multiplies, the infected toenails begin to undergo changes. They may become thickened, brittle, crumbly, and discolored. In more severe cases, the nail can become misshapen and may begin to separate from the nail bed, causing pain and emitting a foul odor. The infection can spread from nail to nail, and surrounding skin can also become infected. A combination of topical and oral medications is often prescribed to treat toenail fungus. Laser therapy can also be a potential treatment option. To learn more, please consult with a podiatrist.
For more information about treatment, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Helping Your Teen Daughter Balance Foot Health and Fashion
You can help your teenage daughter strike a healthy balance between foot health and fashion. Encourage them to wear more supportive footwear (which can still be cute) on a daily basis, while reserving high heels for special occasions. Explain that wearing high heels regularly can damage their muscles and even change their gait. Go over modifications that can help mitigate any damage caused by high heels while still satisfying their desire to be fashionable. For instance, 1 or 2 inch heels can cause fewer foot issues than 4 inch heels. Wider high heels help distribute body weight much more evenly than stilettos, and wider toe boxes avoid toes being squished from pointy or narrow-toed shoes that place excessive pressure on the bones of the foot. When you take them shoe shopping, help them choose footwear that fits well and is comfortable right then and there, rather than buying tighter shoes with the hope of stretching them out at home. Most flip flops do not provide adequate support either and should only be worn getting to and from the beach, in public places that are wet (around pools, in locker rooms and public showers, etc.) and for short periods of time. For more tips on proper footwear and foot care for your teenager, contact a podiatrist.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Mark Isenberg, DPM of Center for Podiatric Excellence. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our office located in Pensacola, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021